Our Diseases
. AMVF Presentation: our aims, how do we operate
2. Our Diseases
3. Medical Research
4. Glossary
5. The AMVF links
6. Help us, Make a donation
2. Our diseases
The liver vessels
The liver is the largest and most important organ of the body with the particular function of permanently processing the blood coming from the digestive system in order to adapt it to the needs of other organs. Like any other organ, it has an artery (input) and hepatic veins (output). But, and this is unique in the whole (of the) body, the liver also has a vein which penetrates it, coming from the intestine, the stomach and the spleen; it is the portal vein.
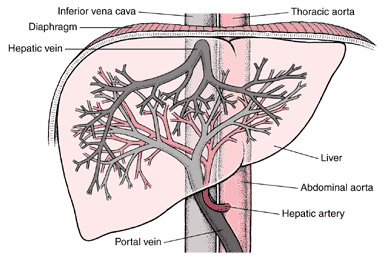
The total blood mass going to and from the liver represents a quarter of the overall blood mass that the heart pumps, (of which a third by the hepatic artery and two thirds by the portal vein).
Attacks of the vessel
The main problems are obstruction of the hepatic veins (Budd Chiari or portal cavernoma) .
In some cases, the obstruction results from a compression due to a nearby injury. Most of the time, the incident is said to be "primitive": thrombosis (blood clot), triggering a phlebitis (venous inflammation).
Thrombosis occurs when blood tends to clot (Prothrombic state) .
Some conditions are inherited, i.e.: like factor V Leiden, factor 2 mutation, shortage of proteins C and S or antithrombin .
Other conditions can appear throughout life, like: myeloproliferative and antiphospholipidic syndromes, nocturnal paroxystic hemoglobinuria, oral contraceptives or pregnancy.
Generally, thrombosis is due to a combination of several factors.
The reasons why thrombosis can occur in the hepatic or portal veins and not elsewhere in the body are still unknown.
Symptoms of our diseases
At the beginning of the thrombosis, patients may have no signs or very common ones.
In some instances, the signs may be very serious:
- extreme fatigue,
- pains, fever,
- abdominal swelling caused by liquid (ascites).
- All intermediate stages are possible.
The initial signs can spontaneously, reduce, disappear or become worse.
Later, the signs reflect the inconvenience of the blood flow in the liver vessels (portal hypertension): abdominal varicose veins, some of which -the oesophageal varicosis- can be the origin of a digestive haemorrhage.
In case of hepatic veins thrombosis, chronic ascites, jaundice, mental confusion, infections will confirm the hepatic functions are affected.
In case of a portal thrombosis, its extension can cause a severe intestine pain.
Nevertheless, even after a very acute start, the effect on the vessels can remain totally invisible. The body has, indeed, some very efficient means to compensate.
EARLY DIAGNOSIS
Early diagnosis can make a difference in our lives.
Quick identification of a vascular disease gives the best chance to identify the causes and then to stop the pernicious impacts to the liver or the intestine;
— to anticipate the extension of the thrombosis to other non-affected veins and even,
— to obtain the regression of certain thrombosis through treatments.
90% of the cases can be diagnosed by non invasive exams (Doppler ultrasound, scan or MRI) which allow the veins to be observed. The results of these exams are all the more trustworthy when the radiologist is well experienced and has been made aware by the physician of the hypothesis of a vascular risk.
Once the diagnosis of the liver vascular disease has been established, specific investigations will be performed by an haematologist to identify the prothrombic status.
Treatments
Treatments exist:
They require the cooperation of experts in several disciplines: specialized labs, hematologists, radiologists, hepatic surgeons, anesthetists, resuscitation specialists and of course hepatologists.
The first step is to:
(a) assess the specific treatment of the causes when they are known;
(b) to administer anticoagulants;
(c) to treat severe manifestations (ascites, kidney failure, infections, digestive hemorrhage)
Nowadays, these treatments are well recognised in liver and gastroenterology units.
The second step is to make the thrombosed veins patent again, once and for all (angioplasty of the hepatic veins or of the vena cava).
In case it fails, the third option is to make a derivation between the portal and the cava systems. This is currently what is done using TIPS. (This technique is far less invasive than surgery).
In case this fails as well, a hepatic transplant must be envisaged.
Thanks to these different treatments, there have been constant improvements in the last thirty years.
Some diseases which were potentially fatal after a few months or years have now become non visible in 85 % of the cases. This is the result of continuous treatment and regular checkups.
The following documents can be downloaded and printed from the links below (updated on 29th of November 2021)
Page précédente : COVID